Lupine Publishers - Journals of Gastroenterology and Hepatology
The Current Approach to the Hepatocellular Carcinoma; AMini Review of Etiology, Prognosis and Treatment by Nuri Emrah Göret in Current Trends in Gastroenterology and Hepatology - Lupine Publishers
Abstract
Keywords: Hepatocellular Carcinoma; Liver Carcinoma; Liver; Cirrhosis
Introduction
HCC can be radiographically diagnosed by computed tomography (CT) or magnetic resonance imaging (MRI). Moreover, dynamic imaging maintains contrast in the early arterial phase, which is then washed or released in the next portal phase. This imaging approach is 90% sensitive and 95% specific for HCC [16]. Ultrasound (US) findings are similar to those of CT and MRI. However, in recent years, contrast-enhanced US is no longer accepted as a diagnostic tool owing to the fact that cholangiocarcinoma cases cannot be distinguished from HCC and further investigation methods are recommended. In terms of laboratory findings, alpha fetoprotein (AFP) elevation in patients with HCC has been known for more than 40 years. AFP elevation can also be detected in pregnancy, normal fetal yolk sac, and fetal liver tissues. Other than HCC, it is also detected in the malignancies of the biliary tract, pancreas, and gastrointestinal system, as well as in nonseminamatous tumors. AFP level is expected to decrease in infants at 300 days after birth, and any AFP elevation detected after this period is a cause to suspect malignancy [17]. However, it has been reported that approximately one-third of the diagnosed cases may have normal AFP levels at the time of diagnosis [18]. Despite the advances in imaging systems and the support provided by laboratory findings, final diagnosis of HCC is still made on the basis of histopathological examination. US or CT-guided cytological fine-needle aspiration biopsy (FNAB) or histological tru-cut biopsy might be preferred in cases suspected with HCC. It has been reported that the diagnostic accuracy of concurrent FNAB and tru-cut biopsy is higher than that of either procedure on its own, with a sensitivity of 96% and specificity of 95% [19]. In microscopic examination of HCC, neoplastic hepatocytes mimic normal liver tissue depending on the degree of differentiation. Well-differentiated tumors that are almost similar to normal tissue are generally difficult to histopathologically distinguish from differentiated liver adenoma tissues. Less differentiated anaplastic tumors can be identified using certain additional immunohistochemical or histochemical analyses because their similarity with normal tissue is reduced.
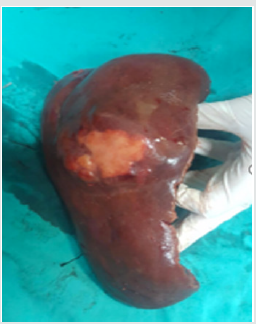
The most common histological patterns in microscopy are trabecular (sinusoidal), solid, and pseudoglandular (acinar) patterns [20]. Most HCC cases are immunohistochemically positive for AFP, epithelial membrane antigen, alpha1 antitrypsin, fibrinogen, IgG, ferritin, Heppar 1, MOC 31, glypican-3, and polyclonal CEA [21]. HCC staging is generally dependent on many criteria such as tumor size, number of tumor nodules, and the presence/absence of vascular invasion [21]. There are various treatment approaches available for HCC cases. Considering the HCC stage, the functional status of liver and the accompanying medical problems, the treatment decision for HCC should be made with a multidisciplinary team comprising a surgeon, oncologist, pathologist, radiologist, and hepatologist [1]. The most effective treatment in HCC cases is surgical resection and liver transplantation (Figures 1 & 2) [22]. Ablative therapies such as radiofrequency ablation (RF), microwave ablation, or percutaneous ethanol injection are among the treatments that should be primarily used for masses smaller than 2 cm. However, ablative therapies are also preferred in patients with advanced age and poor clinical condition, and in whom surgical resection or transplantation cannot be employed [23]. In cases of HCC, many factors such as the number of tumors, tumor size, presence of cirrhosis, and surgical experience should be taken into account before performing resection and transplantation procedures. In case of partial resection of cirrhotic livers, patient’s condition may deteriorate owing to impaired function and low regeneration capacity. For this reason, liver functions should be comprehensively evaluated in patients with cirrhosis, and then decision regarding surgery should be taken [22]. In patients in whom surgery cannot be performed, neoadjuvant therapies such as transarterial embolization (TAE), transarterial chemoembolization (TACE), RF ablation, and percutaneous acid injection can be employed. In addition to these techniques, the use of microwave therapy, transarterial radioembolization, and cryotherapy applications has also been reported. Furthermore, sorafenib, a tyrosine kinase inhibitor used for molecular therapy, can be preferred in patients with advanced stage HCC [24].
References
- Dhanasekaran R, Limaye A, Cabrera R (2012) Hepatocellular carcinoma: current trends in worldwide epidemiology, risk factors, diagnosis, and therapeutics. Hepat Med 4: 19-37.
- Goret CC, Ozkan OF (1978) Primary Tumor of liver; Hepatocellular Carcinoma. Academic Studies in Health Sciences, pp. 249-265.
- Goret CC, Goret NE, Ozkan OF (2019) A Case of Hepatocellular Carcinoma Mimicking Hepatic Adenoma. Ann Ital Chir pii: S2239253X19028895.
- (2011) Surveillance Research Program, National Cancer Institute. Fast stats: an interactive tool for access to SEER cancer statistics.
- Farazi PA, DePinho RA (2006) Hepatocellular carcinoma pathogenesis: from genes to environment. Nat Rev Cancer 6(9): 674-87.
- American Cancer Society. Cancer Facts and FIGS 2005. American Cancer Society.
- Ferlay J, Shin HR, Bray F, Forman D, Mathers C (2010) Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 127(12): 2893-2917.
- Yang HI, Lu SN, Liaw YF, You SL (2002) Taiwan Community-Based Cancer Screening Project Group. Hepatitis B e antigen and the risk of hepatocellular carcinoma. N Engl J Med 347(3): 168-174.
- Colombo M, de Franchis R (1991) Hepatocellular carcinoma in Italian patients with cirrhosis. N Engl J Med 325(10): 675-680.
- Crawford JM (1990) Pathologic assessment of liver cell dysplasia and benign liver tumors: differentiation from malignant tumors. Semin Diagn Pathol 7(2): 115-128.
- Libbrecht L, De Vos R, Cassiman D, Desmet V (2001) Hepatic progenitor cells in hepatocellular adenomas. Am J Surg Pathol 25(11): 1388-1396.
- Smoron GL, Battifora HA (1972) Thorotrast-induced hepatoma. Cancer 30(5): 1252-1259.
- Zhou H, Fischer HP (1998) Liver carcinoma in PiZ alpha-1-antitrypsin deficiency. Am J Surg Pathol 22(6): 742-748.
- Weinberg AG, Mize CE, Worthen HG (1976) The occurrence of hepatoma in the chronic form of hereditary tyrosinemia. J Pediatr. Mar 88(3): 434- 438.
- Alpert ME, Davidson CS (1969) Mycotoxins. A possible cause of primary carcinoma of the liver. Am J Med 46: 325-327.
- Marrero JA, Hussain HK, Nghiem HV, Umar R (2005) Improving the prediction of hepatocellular carcinoma in cirrhotic patients with an arterially-enhancing liver mass. Liver Transpl 11(3): 281-289.
- Bialecki ES, Di Bisceglie AM (2005) Diagnosis of hepatocellular carcinoma. HPB (Oxford) 7(1): 26-34.
- Colombo M (2001) Screening for cancer in viral hepatitis. Clin Liver Dis 5: 109-122.
- Borzio M, Borzio F, Macchi R, Croce AM, Bruno (1994) The evaluation of fine-needle procedures for the diagnosis of focal liver lesions in cirrhosis. J Hepatol 20: 117-121.
- Rosai and Ackerman’s Surgical Pathology (Eds.), (10th edn) I: 944-953.
- Sternberg’s Diagnostic Surgical Pathology (Eds.) (6th edn) II: 736-1739.
- Chedid MF, Kruel CRP, Pinto MA, Grezzana-Filho TJM, Leipnitz I (2017) Hepatocellular Carcınoma: Dıagnosıs And Operatıve Management. Arq Bras Cir Dig 30(4): 272-278.
- Bruix J, Reig M, Sherman M (2016) Evidence Based Diagnosis, Staging, and Treatment of Patients With Hepatocellular Carcinoma. Gastroenterology 150: 835-853.
- Witt Kehati D, Fridkin A, Alaluf MB, Zemel R, Shlomai A (2018) Inhibition of pMAPK14 Overcomes Resistance to Sorafenib in Hepatoma Cells with Hepatitis B Virus. Transl Oncol 11(2): 511-517.
For more Lupine Publishers Please visit our website: https://lupinepublishers.us/
For More Journals of Gastroenterology and Hepatology please visit our website: https://lupinepublishers.com/gastroenterology-hepatology-journal/index.php
For more Open Access Publishers Please visit our Lupine Publishers



Nice post content is impressive to read ,Thanks for proving some helpful information.Hope you will keep on sharing articles.
ReplyDeleteThis provides good insight. You might also be interested to know more about generating more leads and getting the right intelligence to engage prospects. E-Healthcare Lists implements new lead gen ideas and strategies for generating more leads and targeting the right leads and accounts.
E-Healthcare Lists